How Diabetes Impacts Leg Circulation: Key Insights for Prevention and Care
Diabetes, a global health concern, is notorious for its far-reaching effects on various bodily systems, especially the circulatory system. For many, its impact on the legs and feet can lead to life-altering complications. Understanding how diabetes affects leg circulation and learning preventive strategies is vital for patients and caregivers a like.

Understanding the Connection Between Diabetes and Circulation Issues
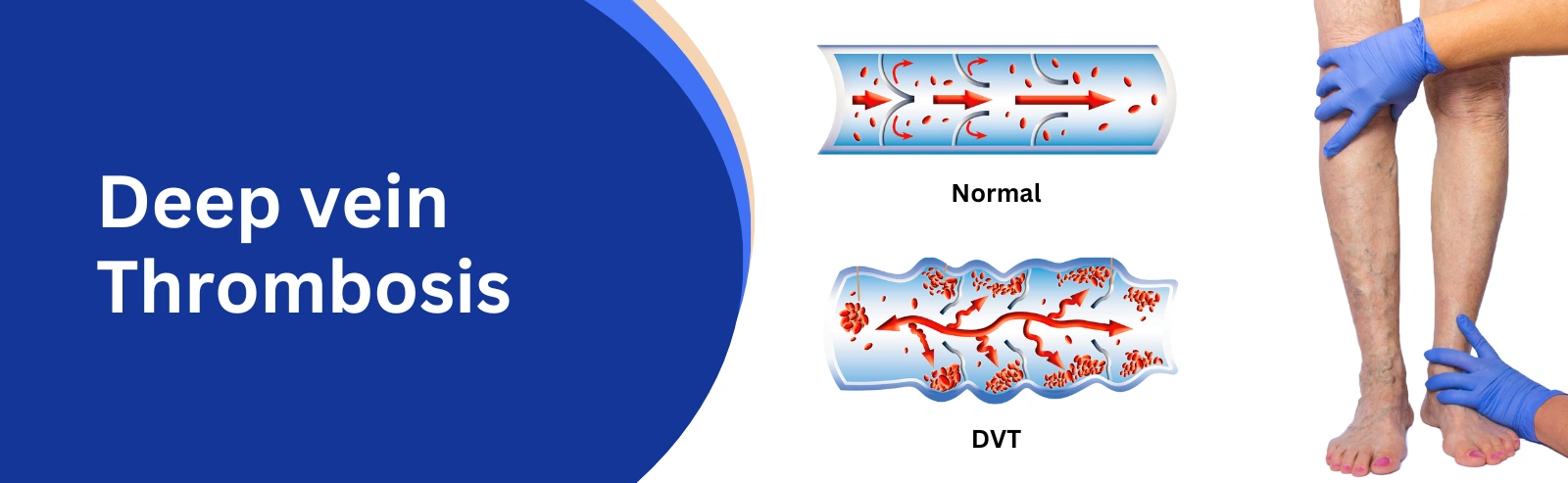
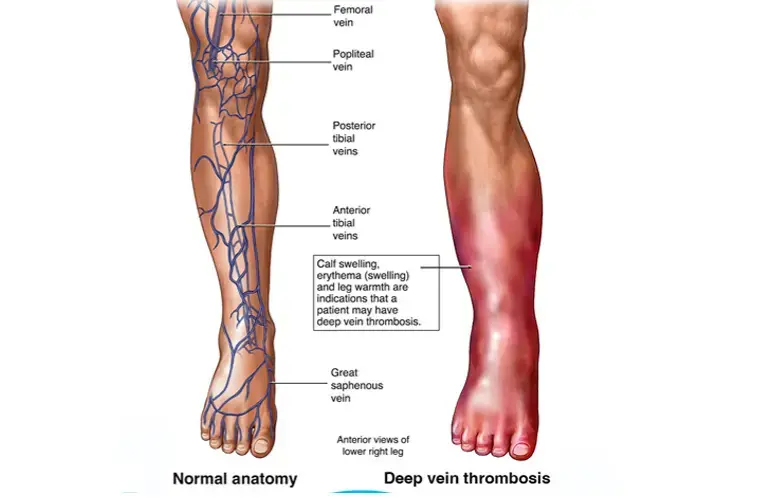
Diabetes elevates blood sugar levels, which can damage blood vessels and nerves over time. This damage significantly impacts circulation, particularly in the lower limbs. Two common issues arise:
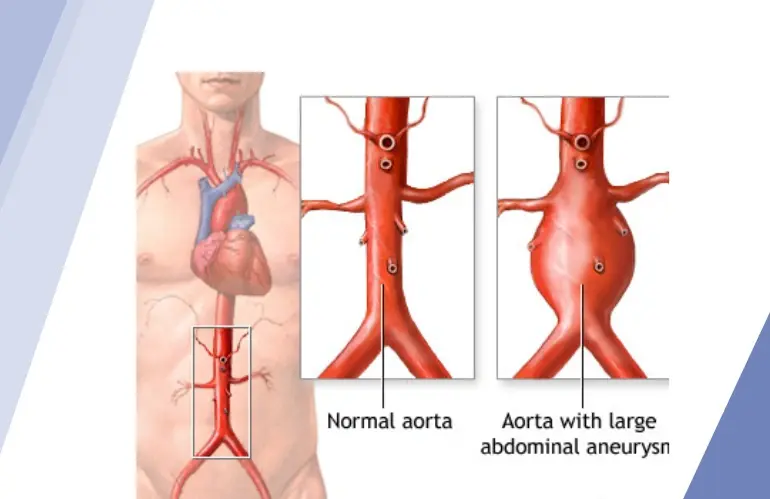
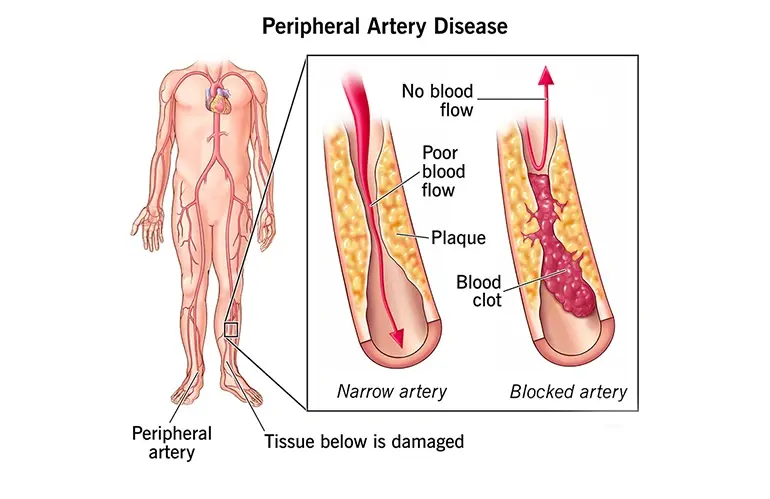
1. Peripheral Artery Disease (PAD): Atherosclerosis, or plaque buildup in the arteries, narrows and blocks blood flow. PAD is prevalent among diabetics and increases the risk of critical limb ischemia and amputations.
2. Diabetic Neuropathy: Nerve damage reduces the sensation in feet and legs, often masking early warning signs of circulation problems until advanced stages.
Symptoms of Poor Circulation in Diabetic Patients
Be vigilant about these common symptoms:
● Cold, pale, or bluish feet and toes.
● Persistent pain, cramping, or heaviness in the legs.
● Wounds or sores that don’t heal.
● Decreased hair growth on legs and toes.
● Loss of sensation or tingling due to neuropathy.
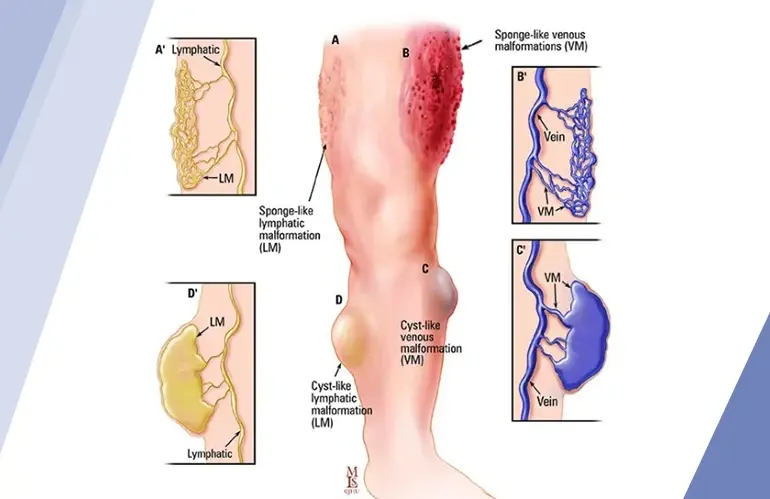
Complications Arising from Circulatory Problems
Unchecked, poor circulation can lead to:
1. Chronic Wounds and Infections: Reduced blood flow hinders the body’s healing ability.
2. Ulcers and Gangrene: Advanced infections can lead to tissue death.
3. Amputations: Diabetes remains a leading cause of non-traumatic lower-limb amputations globally.
Practical Tips to Protect Leg Circulation in Diabetics
1. Control Blood Sugar Levels: Tight glucose management reduces vascular and nerve damage risks.
2. Adopt a Heart-Healthy Diet: Choose foods rich in fiber and healthy fats while avoiding high sugar and saturated fats.
3. Stay Active: Activities like walking, yoga, or cycling improve blood flow and strengthen leg muscles.
4. Quit Smoking: Smoking exacerbates vascular damage, significantly increasing the risk of PAD.
5. Practice Daily Foot Care: Inspect feet daily, wear protective footwear, and moisturize to prevent cracking.
6. Seek Regular Checkups: Routine visits to a podiatrist or vascular specialist can catch problems early.
When to Consult a Specialist
If you notice non-healing wounds, sudden pain, or skin discoloration, consult a vascular specialist immediately. Early intervention can prevent severe outcomes, including amputations.
Conclusion
Managing diabetes effectively and prioritizing vascular health is the key to reducing the impact of poor circulation on your legs. Adopting healthy habits, staying active, and seeking medical care early can make all the difference. Empower yourself with knowledge and take proactive steps today.