Mesenteric Vasculature: Comprehensive Guide to Anatomy and Pathologies
Introduction to Mesenteric Vasculature
The mesenteric vasculature supplies blood to the intestines and includes both arterial and venous systems. Understanding the anatomy and common pathologies affecting this vasculature is crucial for diagnosing and treating conditions that can significantly impact gastrointestinal health.
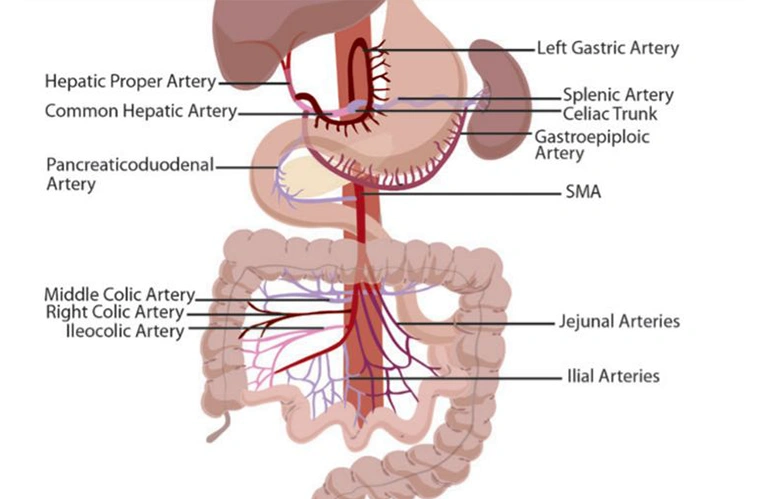
Arterial Mesenteric Anatomy
The arterial mesenteric system comprises the superior mesenteric artery (SMA) and the inferior mesenteric artery (IMA), which provide blood to the intestines.
Superior Mesenteric Artery (SMA)
- Origin: Arises from the anterior surface of the abdominal aorta.
- Branches: Includes intestinal branches, ileocolic artery, right colic artery, and middle colic artery.
- Function: Supplies blood to the small intestine and part of the large intestine.